Chapter 1
Bad Biofilm
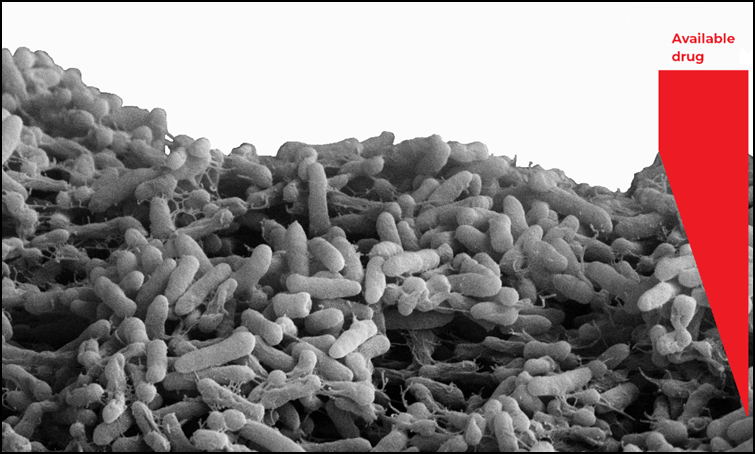
Figure Modified SEM image of simplified mono-species biofilm of Pseudomonas aeruginosa PA01. Schematic representation of drug availability into a biofilm section. The presence of extracellular matrix influences bacteria permeability to drugs. Inside the matrix, efflux pumps and inactivating enzymes reduce the local drug concentration. The amount of drug that escapes these defense mechanisms cannot eradicate biofilm due to the presence of persister cells or small colony variants. Once biofilms are established, bacteria can survive to otherwise lethal treatments, such as UV light, acidity, dehydration, and chemicals. Conventional therapies involving administration of high doses of antibiotic molecules are often insufficient to achieve complete eradication, due to the characteristics of bacteria in biofilms, community structure and resilience [vii,viii].
The most common strategies used to get rid of “bad biofilms” still rely on extensive use of antimicrobial agents (antibiotics, biocides), but the emergence of resistance forces researchers to find new effective strategies to tackle bacterial growth, proliferation, and biofilm formation [i,ii,iii,iv,v,vi].
When researching and developing new antibiotics, the different reaction to therapy between biofilms and planktonic cells cannot be overlooked. Moreover, the toxicological profiles of these incoming approaches need to be carefully investigated before they can enter clinical testing.
- Donlan, R.M.; Costerton, J.W. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 2002, 15(2): 167-193.
- Harrison, J.J.; Ceri, H.; Roper, N.J.; Badry, E.A.; Sproule, K.M.; Turner, R.J. Persister cells mediate tolerance to metal oxyanions in Escherichia coli. Microbiol. 2005, 151(10): 3181-3195.
- Lewis, K. Multidrug tolerance of biofilms and persister cells. Bacterial Biofilms. Curr. Top Microbiol. Immunol. Berlin, Heidelberg: Springer. 2008, 322:107-131.
- Römling, U.; Balsalobre, C. Biofilm infections, their resilience to therapy and innovative treatment strategies. J Intern med. 2012, 272(6):541-561.
- Da Silva, A.C.B.; Stipp, R.N.; de Oliveira Mattos-Graner, R.; Sampaio, F.C.; de Araújo; D.A.M. Influence of sub-lethal and lethal concentrations of chlorhexidine on morphology and glucosyltransferase genes expression in Streptococcus mutans UA159. Adv. Microbiol. 2014, 4(13): 945.
-
Conlon, B.P.; Rowe, S.E.; Lewis, K. Persister cells in biofilm associated infections. Biofilm-based Healthcare-Associated Infections. Springer, Cham. 2015, 1-9.
-
Lebeaux, D.; Ghigo, J.M.; Beloin, C. Biofilm-related infections: bridging the gap between clinical management and fundamental aspects of recalcitrance toward antibiotics. Microbiol. Mol. Biol. Rev. 2014, 78(3):510-543.
-
Trombetta, R.P.; Dunman, P.M.; Schwarz, E.M.; Kates, S.L.; Awad, H.A. A High-Throughput Screening Approach To Repurpose FDA-Approved Drugs for Bactericidal Applications against Staphylococcus aureus Small-Colony Variants. mSphere. 2018, 3(5):e00422-18.